- Home
- Medial Patellofemoral Ligament Reconstruction
Medial Patellofemoral Ligament Reconstruction
The Medial Patellofemoral Ligament (MPFL) Reconstruction
The Medial Patellofemeral Ligament (MPFL) attaches the kneecap (patella) to the inner part of the knee. It helps stabilize the kneecap as the knee moves, preventing it from moving or dislocating outward.
CAUSES
The MFPL is most commonly injured when the kneecap is dislocated. Patients with an underlying abnormality of the knee, ligament laxity or weak leg muscles are at an increased risk for patella dislocations. Individuals who play sports or are involved in activities that involve pivoting are also at high risk.
TREATMENT
Most first time MPFL injuries can be treated non-surgically with NSAIDs and immobilization. It’s then followed by physical therapy to strengthen the muscles around the knee. Your physician may recommend surgery if the injury is more severe, or if there are small pieces of detached bone or cartilage in the knee. MFPL reconstruction is often recommended for patients who experience repeated kneecap dislocations.
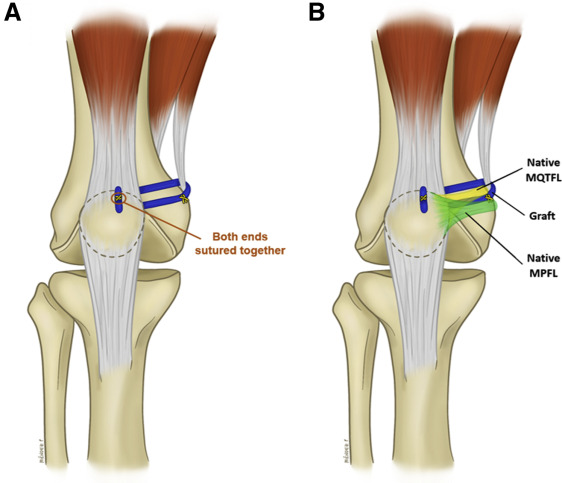
Depending on the patient’s individual condition, knee surgeons will either directly repair the ligament, or reconstruct the ligament. Surgeons will use a graft from another ligament in the patient’s own body or with that of a donor. This will provide stabilization to the knee and will allow the patient to return to normal activity.
Typically, MPFL reconstruction is performed at an outpatient facility. The knee will be immobilized while walking and standing for a period of six weeks, followed by a program of physical therapy. Patients usually return to normal activity after a period of four to six months.
BOOK AN APPOINTMENT
“KNEEO Technique” For Knee Replacements
Injury to the MPFL
In the healthy knee, the bones that make up the patellofemoral joint move smoothly against one another as the joint is flexed or extended. The patella glides in a trochlea (groove) of the femur. The MPFL plays a particularly important role in keeping the patella on track (that is, in this groove) by acting like a leash that restrains the patella’s movement.
When patellar dislocation occurs, soft tissues are damaged as the patella “jumps” the track and then comes forcibly back into place. Because the kneecap dislocates toward the outside of the leg, the ligament on the inside of the knee (the MPFL) gets torn.
Left untreated, an injured MPFL can heal on its own. However, when left alone, the ligament heals in a loosened, lengthened position. This causes instability that makes it easier for the patella to become dislocated again in the future. This, in turn can cause damage to the cartilage in the knee. While the pain, swelling and disability associated with a dislocated kneecap are problems in themselves, the greater concern is subsequent injury to the cartilage that covers the ends of the bones where they meet in the knee joint. Once this cartilage is damaged, you are put at a high risk of developing patellofemoral arthritis, a significantly more difficult condition to treat. For this reason, it always advisable to get treatment that will help prevent further dislocations of the kneecap.
MPFL reconstruction protocol
At the Patellofemoral Center at HSS, patients with patellar instability undergo a thorough assessment that includes a physical examination and review of the patient’s medical history. A magnetic resonance imaging (MRI) is also performed to help the doctor understand the condition of the cartilage in the patellofemoral joint and helps determine whether the patient is a candidate for MPFL or a bony procedure, such as tibial tubercle transfer. Often, these images can be obtained on the same day as an initial visit.
Although non-operative treatment does not have a significant role in the treatment of patellar instability, if the patient has experienced a single dislocation without a cartilage injury on MRI he or she will be treated with short term immobilization and physical therapy. Almost all candidates for MPFL reconstruction have dislocated their knee more than once, and in some cases may have experienced multiple dislocations. (MPFL may be performed in a patient who has had single dislocation, but only in the presence of other problems in the knee that also require surgical intervention.)
Patients undergoing MPFL reconstruction receive regional anesthesia – an spinal nerve block that numbs the lower half of the body – and sedation. The orthopedic surgeon then replaces the injured ligament with a portion of a tendon taken either from the patient’s own hamstring or from donor tissue. An arthroscope is used to view the surgical area, and the ligament reconstruction is conducted using two small incisions. The entire surgery takes about an hour, and patients return home the same day, with their knee stabilized in a brace.
MPFL reconstruction produces excellent results and has a very low rate of complication. Rare complications can, however, include fractures, infections or blood clots. The procedure can be performed safely in children with open growth plates (the area where bone grows), as opposed to surgical approaches that change bone alignment and which are not appropriate in young patients. With no alternative available, in the past, children were sometimes placed in a brace, but remained at risk for additional dislocations until they reached skeletal maturity, at which time a surgical reshaping of the bone (osteotomy) would become an option. Today, MPFL reconstruction is a safe option for children and teenagers.
In rare cases, people with patellar instability may be candidates for a surgical repair of their MPFL, rather than a complete MPFL reconstruction, such as when the MPFL has pulled a small piece of bone off the inside part of the kneecap.


