- Home
- Meniscal Transplant
Meniscal Transplant
Meniscal Transplant Surgery
The meniscus is a C-shaped cushion of cartilage in the knee joint. When people talk about “torn cartilage” in the knee, they are usually referring to a torn meniscus. If the meniscus is so badly damaged that it cannot be repaired, it may need to be removed or trimmed out. This is called a partial meniscectomy and is often effective in relieving the pain of a meniscus tear. When the meniscus is largely gone, however, persistent knee pain and or osteoarthritis can develop. For many older patients with this condition, a total or partial joint replacement might be the right option. But active people who are younger than 40 may be eligible for an alternative treatment: meniscal transplant surgery.
Anatomy
Three bones meet to form your knee joint: your thighbone (femur), shinbone (tibia), and kneecap (patella). The ends of your thighbone and shinbone are covered with articular cartilage. This slippery substance helps your knee bones glide smoothly across each other as you bend or straighten your leg. Two wedge-shaped pieces of meniscal cartilage act as “shock absorbers” in the knee joint. Different from articular cartilage, the meniscus is tough and rubbery to help cushion and stabilize the joint. Each knee has two menisci, one on each side of the joint. If your meniscus is severely damaged or has been removed, the articular cartilage protecting your knee may begin to wear, similar to how rubber on a car tire wears away over time. As this cartilage wears away, it can lead to pain and disability. This condition is called osteoarthritis. The goal of meniscal transplant surgery is to replace the meniscus cushion before the articular cartilage is damaged. The donor meniscus is intended to take the place of the native meniscus, relieve knee pain, and prevent the progression to osteoarthritis.
BOOK AN APPOINTMENT
“KNEEO Technique” For Knee Replacements
Patient Eligibility
Although meniscal transplants have been performed for more than 20 years, the procedure is still relatively uncommon. This is largely due to the strict criteria patients must meet to be considered for the procedure.
Most people with severe meniscal problems have also developed arthritis in the knee. If the articular cartilage has worn away too much, a meniscal transplant will not be helpful.
The criteria for meniscal transplant include:
- Younger than 40-45 years and physically active
- Missing a significant portion of the meniscus as the result of previous surgery or injury
- Persistent activity-related pain
- Knee with stable ligaments and normal alignment (alignment issues can also be corrected at the time of the transplant with a procedure called an “osteotomy”)
- No or minimal knee osteoarthritis and no rheumatoid arthritis
- Not obese
Surgery
Meniscal transplant surgery is an arthroscopic procedure that usually needs one or two small incisions. It is typically performed on an outpatient basis.
Procedure
Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. He or she then inserts surgical instruments through other small incisions to perform the procedure.
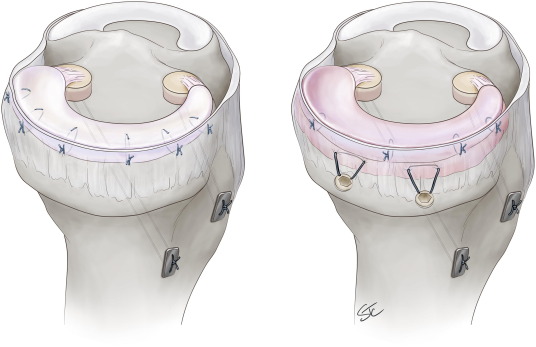
The new meniscal tissue is anchored into the shinbone to stabilize the transplant. More stitches are placed into the meniscal transplant to sew it into place and attach it to the knee capsule.
Surgical Complications
The risk of complications from meniscal transplant surgery is very low. Stiffness, reoperation, and incomplete healing are the most common complications.
Other risks include bleeding, infection, and damage to nearby nerves or blood vessels.
The risk of getting an infection from donor tissue is extremely low.
Rehabilitation
Immobilization. You will need to wear a knee brace and use crutches for the first 4 to 6 weeks after surgery. This gives the transplanted tissue time to become firmly attached to the bone. Range of motion is typically initiated as soon as possible after the procedure.
Physical therapy. Once the initial pain and swelling have settled down, physical therapy can begin. Physical therapy initially focuses on pain management, muscle reactivation, and motion. Gentle stretches will improve range of motion. As healing progresses, strengthening exercises will gradually be added to your program.
Return to daily activities. Most patients are not able to return to work for at least 2 weeks after surgery. Patients with active or labor-intensive jobs may require 3 to 4 months of rehabilitation before they return to work. Your doctor will talk with you about when it is safe to return to work. Full release for sports activity is typically given 6 to 12 months after surgery.


