- Home
- Treatment for Discoid Meniscus
Treatment for Discoid Meniscus
Treatment of Discoid Meniscus
There is a greater incidence of discoid meniscus in Asian countries than in Western countries, and bilateral discoid menisci are also common. The discoid meniscus may be a congenital anomaly, and genetics or family history may play a role in the development of discoid menisci. Because the histology of discoid meniscus is different from that of normal meniscus, it is prone to tearing. Individuals with a discoid meniscus can be asymptomatic or symptomatic. Asymptomatic discoid menisci do not require treatment. However, operative treatment is necessary if there are symptoms. Total meniscectomy leads to an increased risk of osteoarthritis. Therefore, total meniscectomy is generally reserved for rare unsalvageable cases. Partial meniscectomy (saucerization) with preservation of a stable peripheral rim combined with or without peripheral repair is effective, and good short-, mid-, and long-term clinical results have been reported.
Introduction
The discoid meniscus was first observed in a cadaver specimen by Young in 1889. For many years, the discoid meniscus was considered to be synonymous with snapping knee syndrome, which was first described by in 1936. The incidence of discoid lateral meniscus is estimated to be 0.4% to 17%, whereas the discoid medial meniscus is extremely rare (0.1% to 0.3%). It has been reported that about 20% of cases are bilateral. However, the true incidence and prevalence are unknown, given that many asymptomatic discoid menisci are incidentally discovered during surgery. Some authors have reported that magnetic resonance imaging (MRI) or arthroscopic evaluation reveals higher rates (79% to 97%) of bilateral discoid lateral meniscus in patients presenting with symptomatic unilateral discoid lateral meniscus. There is a greater incidence of discoid meniscus in Asian countries than in Western countries. Fukuta et al. reported an incidence of 13% in Japan, Kim et al. observed an incidence of 10.6% in Korea, and Rao et al. noted an incidence of 5.8% in India. In contrast, Jordan described an incidence of 3% to 5% in the United States. This review summarizes the current knowledge on the diagnosis and treatment of discoid meniscus.
BOOK AN APPOINTMENT
“KNEEO Technique” For Knee Replacements
Treatment
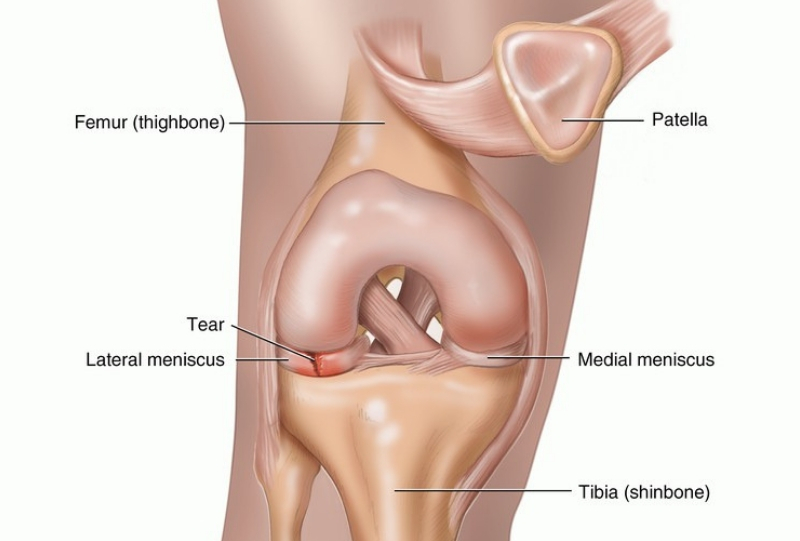
The factors determining treatment include the type of discoid meniscus, concomitant symptoms, duration of symptoms, and age. Most cases of discoid meniscus remain asymptomatic and do not require treatment, even when snapping is present because the knee may have adapted to the discoid anatomy and continues to function well. However, there is some debate about the need for treatment in cases of asymptomatic, stable discoid meniscus found incidentally during evaluation or treatment of some other knee conditions. If there are symptoms such as pain, locking, swelling, giving way, or instability, it is necessary to operate. In the case of a symptomatic but stable meniscus, some authors have suggested total meniscectomy due to the risk of intrinsic abnormalities in the remaining meniscal tissue. However, many studies have suggested that total meniscectomy leads to a high risk of osteoarthritis. Total meniscectomy is generally avoided in children, except in rare cases in which the entire meniscus is deemed to be unsalvageable. Partial meniscectomy (saucerization) with preservation of a stable peripheral rim, with or without peripheral repair, is effective and has been recommended by many authors. For the unstable type, repair of the posterior tibial detachment is important to eliminate the risk of osteoarthritis after total meniscectomy.
Arthroscopic partial meniscectomy (saucerization) is most commonly recommended. This treatment attempts to change the meniscus to a more normal shape and size. In cases of peripheral tear in the vascular zone, arthroscopic meniscal repair can be done with saucerization according to advancement of the repair technique. The goal of saucerization is to create a stable and functional meniscus that will provide adequate shock absorption without retearing. Many authors have recommended that at least 6 mm to 8 mm from the periphery should remain; however, larger meniscal remnants after saucerization have been associated with increased re-tear rates.
After partial meniscectomy (saucerization) and/or repair of a discoid meniscus, the remaining discoid meniscus is more vulnerable to tearing than the normal meniscus because the cartilage remains thickened due to the abnormal discoid meniscus. A complication unique to discoid meniscus surgery is osteochondritis dissecans (OCD) of the lateral femoral condyle, which can occur after total or partial meniscetomy of the discoid lateral meniscus. Repeated impaction in the immature chondral structure after resection of the discoid meniscus might predispose to the development of OCD in the lateral femoral condyle. In addition, the change of alignment to valgus after resection of a thick discoid meniscus can lead to concentrated stress on the lateral femoral condyle.


